The 1918 Spanish flu pandemic was the
deadliest of all modern pandemics, killing 17-50 million people from February 1918 to April 1920.

One of the interesting factors of the Spanish flu, as it is known today, is that viruses were too small to see
with the microscopes of the day, so people were
not even aware that viruses existed.
What they were able to find in patients back then, to link the entire pandemic together,
was bacillus influenzae
– the bacteria of influenza, which was believed to be the cause
of influenza until the 1930’s. Some recent research found that most of the 'Spanish flu'
deaths were, as diagnosed at the time, due to these
bacterial superinfections,
which
themselves can be exacerbated by any illness weakening the body.
So, it is possible that deaths attributed over two entire years to the 'Spanish flu' could
have been from a wide range of illnesses that
result in pneumonia, including coronavirus colds, etc.
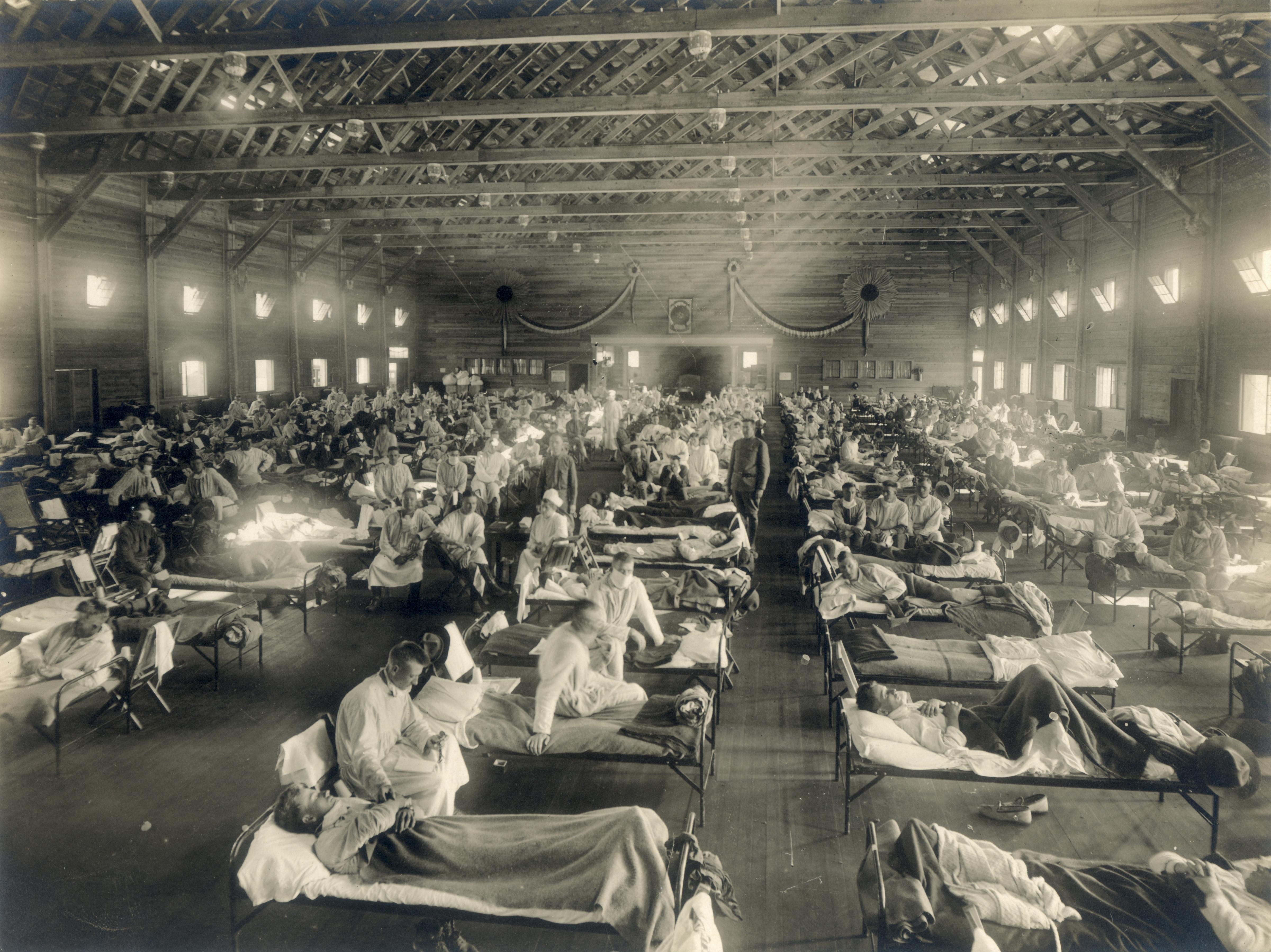
Bacterial infections require close-quarters with other
infected individuals - almost like in the famous photos of open-air warehouses
filled with beds, in which patients would cough up
into the air, and all-over other patients.
As patients died of the bacterial infection they got at the hospital,
those newly empty beds would be filled with new patients suffering from cold or flu,
who would've otherwise recovered in a week or so at home,
only to be infected with bacteria from the patients next to them that would make them sicker,
and eventually kill them, thus opening up that bed for the next patient.
The first wave
of the 1918 pandemic,
in March-June 1918, traditionally cold season,
caused only a mild elevation in what was reported as “flu-related deaths".
The second wave in
September-December, traditionally flu season, saw deaths at a level that could easily
be described
as a different disease, and strangely, seemed to affect young people more than the
usually vulnerable old.
The third wave was from January-June 1919, again, traditionally cold season,
and behaved differently than the second wave -
closer in deadliness to the first wave, only slightly more so. A fourth wave,
again, more minor, and in cold season,
was seen in some places in January-March 1920.
A few preserved samples from the most-deadly, and therefore, most studied, second wave,
were later positively identified as having an influenza virus infection.
However, given that bacteria was the presumed cause throughout this time,
and the reason we think of these two entire years as one pandemic 'event'
is because of the way it was recorded and taught, one possible view of
these different waves, is that each was driven by a different disease -
a cold, the identified flu, a cold, and then a cold, in turn.
We then assumed that they were all the same disease, both because it was similarly
'bad' throughout this period, and because that was the prevailing view after most
of those dying were found to have the same bacteria, by the microscopes they had available at that time.
But what if other factors
led to a series of bad airborne diseases over those two years?
It is possible that the first 1918 season's 'bad cold' set off a wave of
virus-avoidance behavior in communities, which was then fully
in force by the second wave.
If people were frightened into believing that there was a 'super-illness'
going around, particularly
in younger individuals who
hadn't seen bad cold seasons before, they would feel that the thing to do
was to crowd into hospitals for treatment, where they would
then be exposed to the bacterial infection that would kill them.
Interestingly, China was hit by this second wave flu, but for them,
it was a mild season,
and they did not experience the level of deaths
seen elsewhere around the world, suggesting that even that second wave flu was just an ordinary flu,
with nothing special about it except
the virus-avoidance behavior of much of the world in dealing with it.
The virus-avoidance culture, and associated hysteria driving people to the hospital,
then began to dissipate after the third ‘bad cold’ wave, leading to less impactful
airborne illnesses.
As always, there would be many contributing factors to overall health results - another possible contributor
to the deadliness in 1918 was the level of pollution in a newly industrialized
world. This was decades prior to emissions controls, and it was difficult to see across the street in many cities
across the United States. So, there was likely a much larger vulnerable population to respiratory disease worldwide
back then, similar to what we see in Covid-19 deaths in countries like Thailand,
with high levels of pollution.
It is difficult to know for sure what had happened in the past,
particularly when all the types of evidence we might consider today,
were not available back then. But one thing is for sure: when human
observation is the lens through which an event is seen, it is always
helpful to question whether the prevailing view is built upon a
chain of misconceptions.
While there are many reasons why humans are often incapable of admitting
mistakes,
one of the biggest indicators that the
response to the Spanish flu was considered to be a failure by those who
lived through it, was in survivors of the Spanish flu
who led the response to pandemics
several times more deadly than Covid-19
in the 1950's and 1960's, who rejected
Virus-Avoidance Strategies.